THIS INFORMATION IS ONLY FOR THE USE OF PARENTS AND PATIENTS OF GLENDALE PEDIATRICS
We at Glendale Pediatrics are always available to answer your concerns about your child. The following information is a set of guidelines to help you with decision-making regarding your ill child. Please do not hesitate to contact us or to seek medical attention if after reading the information below, you are still uncertain of what to do, or if your gut instinct is telling you that your child is not OK.
- Head Injuries
- Hives
- Lice
- Painful Urination
- Pink Eye (Conjunctivitis)
- Sore Throat
- Teething
- Testicular Pain
- The Common Cold/Cough
- The Flu (Influenza)
- Vomiting
- What if I need a refill of a prescription?
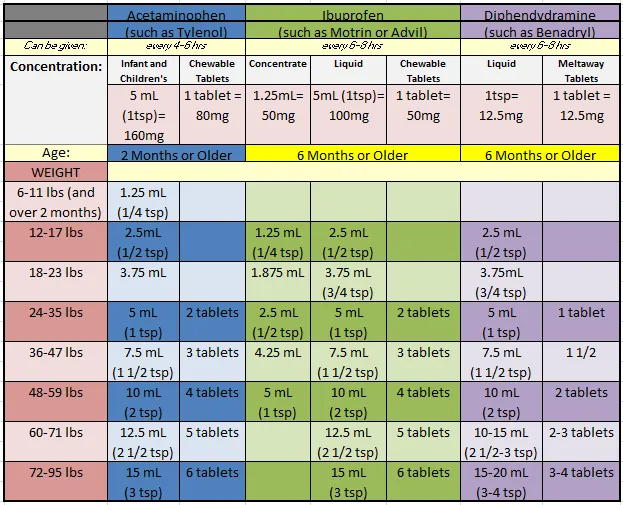
Dosage Chart
When giving your child medications, it's important to check the concentration (this means HOW MANY MILLIGRAMS PER UNIT OF MEASURE) of the medication you are using. Our chart lists medications by concentration. If you have any questions regarding which concentration you have and how to dose it, please speak with your pharmacist or call our office.
See package directions for older children.
We generally do not recommend use of multi-system cough or cold medications in children, particularly in children under the age of six.
Fever
Fevers are helpful!
Fever is an important tool our bodies use to help us fight off more serious infection. Many parents worry that fever is harmful, but fever is actually helpful in preventing more serious illness. Normal fevers of 100-104 are actually good for children (exception in infants under two months of age), and higher fevers over 104 that our bodies generate do not cause brain damage. In general, your child’s symptoms and how sick your child looks and acts is much more important that the actual temperature (exception to this includes infants under 2 months of age and immunocompromised individuals). Fever is defined as: rectal, forehead or temporal artery temperature of 100.4 (38 C) or higher under the tongue temperature of 100 (37.8) or higher armpit temperature of 99 (37.2) or higher - note: this tends to be an inaccurate way to measure ear temperatures tend to be inaccurate in children A few facts about fever: Fever is your body’s way of fighting against serious infection. Many febrile illnesses in kids are viral. When we get a fever with a viral infection, our body is trying to prevent bacterial growth/infection. Fevers with infections don’t cause brain damage. Fevers from being in very hot air temperature can cause brain damage and require immediate medical attention (heat exhaustion or heat stroke). High fever doesn’t cause a seizure. About 2-4% of children under 6y can have seizure with fever. These seizures, while frightening to watch, generally last less than five minutes and do not cause permanent harm. Febrile seizures require a discussion with your physician. High fevers do not be treated or brought down. Sometimes kids can look very sleepy and out of it when they have a higher fever, but this resolves when the fever comes down. In general, treat with acetaminophen or ibuprofen for misery or discomfort or if you are trying to understand if your child is truly lethargic. Said another way, if your child is very sleepy or out of it with a fever, please give ibuprofen or acetaminophen and reassess in 30-60 minutes. If they remain lethargic at that time, they require evaluation. Fever will go up and down throughout the day. Commonly, kids will have highest fevers in the late afternoon and night. Fever is generally thought to be resolved once your child has had 24h without fever without use of a fever-reducer.
What you can do
Children under two months of age:
In infants under 2 months, any fever is concerning and requires immediate medical attention. Infants should have their temperature taken rectally only - other methods are not accurate. Make sure your baby isn’t overdressed, as this will sometimes raise the temperature. Do not give any fever reducer to children under 2 months of age. Infants can also be very ill without having a fever - if your child is lethargic or sleepy (eg. you are unable to wake the baby for 2 feedings in a row) or irritable (eg. you are unable to console your baby despite a variety of attempts) or is having difficulty breathing or just doesn’t look or seem right to you, you should call your doctor immediately.
Children over two months of age:
Remember, fever is one of the good guys, so don’t suppress it unless your child is miserable or in pain. You may administer acetaminophen (Tylenol) or, if your child is over 6 months of age, ibuprofen (Advil) for pain or discomfort.
IMPORTANT: NEVER USE ASPIRIN FOR CHILDREN UNDER 18 YEARS OF AGE!
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- is extremely irritable or lethargic and does not improve after acetaminophen or ibuprofen.
- has difficulty breathing.
- has a stiff (not sore) neck.
- has a spreading purplish rash.
- has a seizure (convulsion). If your child has a seizure that lasts more than 5 minutes, call 911.
- has a temperature over 105.5 taken rectally (note: this does not necessarily mean a more serious illness, though).
CALL DURING OFFICE HOURS IF YOUR CHILD:
- is not improving after 48-72h of fever.
- is becoming increasingly fussy.
- you are concerned.
- is irritable or lethargic and does not improve after Tylenol or Motrin and a tepid bath.
- has difficulty breathing.
- has a stiff (not sore) neck or a spreading purple rash.
- has a seizure (convulsion). If your child has a seizure that lasts more than 5 minutes, call 911.
- has a temperature over 105 taken rectally.
Call during office hours if your child:
- is not improving after 48 to 72 hours of fever.
- is becoming increasingly fussy.
- you are concerned.
Bee and wasp stings are painful initially and become itchy and swollen over subsequent days. Bees sting only if provoked or touched, such as if they are stepped on or picked up. Wasps can be aggressive and can sting more than once. Bees die when they sting because their stinger and venom sac are left behind, whereas wasps do not lose their venom sac when they sting. Getting the stinger out quickly will decrease the amount of venom that gets released into the skin, minimizing potential reaction.
What you can do
- look carefully to see if there is a stinger and/or sac left at the sight of the sting. If there is, carefully remove it by scraping over it with a credit card or your fingernail. Never use tweezers to remove a stinger because more venom can be released into the skin.
- wash the area carefully with soap and water.
- apply cold pack in short intervals to minimize swelling. You may also elevate the area of the sting.
- consider giving a pain reliever such as ibuprofen or acetaminophen or an antihistamine such as cetirizine (Zyrtec) to decrease itching.
- the site may become very swollen and itchy over the subsequent days.
CALL 911 IF YOUR CHILD:
- has difficulty breathing or hoarseness.
- has generalized swelling.
- has swelling around the mouth.
- loses consciousness or has weakness.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- develops hives.
- develops a wheeze or cough.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- your child develops swelling associated with tenderness or a fever in the days after a bee sting.
BLOODY NOSE
Bloody noses are common. They occur frequently when the weather is hot and dry, if the heater is on or during colds or with allergies. Some kids are more prone to bloody noses than others.
What you can do
- sit up and lean forward.
- squeeze the lower half of the nose (the entire nose below the nasal bone that can be squeezed flat, not just the tip or the ends of the nostrils). Hold for a full 5 minutes before checking!
- if the bleeding doesn’t stop, hold for 10 minutes before checking.
- about an hour after the nosebleed, push a small amount of antibiotic ointment, nasal saline gel or petroleum jelly (Vaseline) into the nostril, then gently squeeze the nostrils and wipe off excess.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- doesn’t stop bleeding after 30 min of continuous pressure or is bleeding profusely despite the above measures, especially if associated with feeling lightheadedness or looking paler than usual.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- has frequent nose bleeds that are difficult to manage.
BRONCHIOLITIS
Bronchiolitis is a viral respiratory infection of the small airways of the lung, causing swelling and mucus production. It commonly leads to breathing problems in kids under 2 years of age. The most common cause is infection with respiratory syncytial virus (RSV), but other viruses can also cause bronchiolitis.
Symptoms include fever, runny nose, congestion, cough, wheezing, faster breathing and noisy breathing. Symptoms typically peak on days 3-7. The cough can last for 4 weeks or more.
Diagnosis of bronchiolitis is primarily based on medical history, symptoms and physical exam - no special testing is required. We are currently only able to treat the symptoms of bronchiolitis, not the infection itself.
What you can do
- Clear the nose! One of the worst things for kids with bronchiolitis is thick nasal congestion. Have your child blow their nose. If they are too young to do so, you may put a few drops of saline in one nostril, wait a few seconds and then suction with a bulb syringe or Nose Frida. This is especially important before eating and sleeping.
- Keep hydrated. Offer plenty of fluids throughout the day.
- Elevate the head and upper body, especially during feedings.
- Humidify the air to help thick mucus to drain.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- has difficulty breathing or fast breathing not relieved by clearing the nose. The is especially important if your child is breathing faster than 60 breaths per minute or looks like they are having to work hard to breathe - retracting under the ribs or between the ribs, using the belly to breathe, nasal flaring, grunting with breaths, head bobbing.
- is unable to keep hydrated because of trouble breathing.
- looks pale or has blue color to fingernails/toenails, nose or lips.
- stops breathing for more than 10-20 seconds.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- seems to be having milder difficulty with breathing.
- fever persists longer than 3 days or the fever goes away and recurs.
- you are concerned.
BURNS
Burns are heat, friction or chemical injuries of the skin. The injury can range from mild redness to severe injury through all layers of the skin. The full extent of a burn is not known at the time of the injury. A burn can begin as a red spot and develop blisters minutes to hours later.
What you can do
Thermal burns:
- immediately run cold tap water on the burn and rip off any overlying clothing including diapers.
- cool the burn with cold tap water or rotating wash cloths or gauze soaked in ice water for 15-30 minutes continuously. This can decrease the pain as well as the depth of the burn. Even if the burn looks terrible, start the cooling process first before making your next decision.
- after cooling, if blisters are not broken, gently wash them and apply antibiotic ointment and a dressing to protect the blisters.
- if blisters are open, wash the area gently and carefully remove the cover of the broken blister and apply a generous amount of double antibiotic ointment and a sterile gauze until it can be evaluated in the office.
- re-dress daily.
Friction burns:
- gently clean out all of the dirt, gravel and sand to avoid a tattoo effect when it heals.
- wash gently and thoroughly.
- apply a generous amount of double antibiotic ointment and cover with gauze.
- re-dress daily.
CALL 911 IF YOUR CHILD:
- was burned in a fire and has coughing and/or breathing or possible smoke inhalation.
- the burn covers a large area of the body.
- your child has other generalized symptoms, such as weakness, difficulty breathing or altered level of consciousness.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- the burn is large and you are unsure if you need to go to the hospital.
- your child is in considerable pain despite 40-60 minutes of cooling and a dose of ibuprofen.
- your child has a fever.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- has a burn over a joint.
- has a burn of moderate size with either intact or open blisters.
- the burn is not healing.
- you are having difficulty dressing or cleaning the wound.
- you notice any pus discharge from the wound.
THE COMMON COLD
A cold is an infection caused by a virus, leading to nasal congestion, runny nose, cough, and occasionally fever, sore throat and watery eyes. There are thousands of different viruses causing upper respiratory tract infections, and young kids can get one new cold after another in the winter. Colds usually get worse for the first 48-72h before they begin to improve. Runny nose tends to become yellow or green after the first 2-3 days and can last for up to two+ weeks. Antibiotics do not help with or prevent colds.
What you can do
- Elevate the head.
- Clear the nose - have your child blow the nose. If they are too young to do so, you may put a few drops of saline in one nostril, wait a few seconds and then suction with a bulb syringe or Nose Frida.
- Do not use over-the-counter cough or cold medicines if your child is under 6y.
- Do not use antihistamines unless your child has allergies.
- You can help soothe a cough by using a homeopathic or honey-containing syrup. Do not use honey in children under one year of age.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- has difficulty breathing that is not improved with nasal suction and elevating the head.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- has green or yellow nasal discharge that lasts more than 2 weeks.
- has congestion lasting more than 2-3 weeks.
- ear pain.
- fever lasting more than 3 days.
CONSTIPATION
Constipation is defined as hard or painful bowel movements. Children do not have to have daily bowel movements, though most should. The consistency of the stool and the effort required to pass the stool is more important than the frequency of bowel movements. Some breast-fed infants may start having infrequent bowel movements around six weeks of life, and may occur as infrequently as weekly. This can be normal as long as the stools are still loose and unformed in consistency.
Constipation needs to be treated if:
- stools are very firm, hard or pellet-like.
- your child has difficulty passing stools.
- your child is bloated or having abdominal pain due to constipation.
- you notice decreased appetite or nausea related to constipation.
- you see blood in the stool or when wiping.
- your child is trying to hold stools secondary to pain or discomfort.
- your child is having stool accidents related to withholding (called encopresis).
What you can do
For infants under one month:
- increase feedings. Do not give water.
- if your baby is comfortable and stool is soft consistency, ok to continue to monitor.
- if your baby is gassy or pushing, try bicycle leg exercises or tummy massage.
- if your baby continues to be uncomfortable, stimulate rectum by inserting a vaseline-coated Q-tip or thermometer only about one centimeter (about 1/2 inch) into anus and turning the Q-tip about 3-4 times. Do not do this repeatedly.
For infants 1-6 months:
- it may be normal to not stool for about a week. Seek medical attention if the baby’s belly is distended or the baby is having pain.
- consider adding 1 tsp sugar or 1/2-1 oz pear juice to 4 oz expressed breast milk or formula.
- do not give water until the baby is at least 4 months old.
- babies over 4 months may take 2 oz of prune, plum or pear juice diluted with 2 oz water per day. You may also offer pureed prunes or other stone fruits.
- if your baby is gassy or appears to be pushing, try bicycle leg exercises or tummy massage.
- if your baby continues to be uncomfortable, stimulate rectum by inserting a vaseline-coated Q-tip or thermometer only about one centimeter (about 1/2 inch) into anus and turning the Q-tip about 3-4 times. Do not do this repeatedly.
- consider adding an infant probiotic, such as Gerber Soothe or Culturelle.
- consider changing formula (consider Enfamil Reguline or Gerber Good Start).
For older infants and children:
- try prune, plum or pear juice diluted with equal parts water.
- increase water intake.
- increase intake of high fiber fruits and vegetables, such as stone fruits (peaches, plums, mango, apricot), pears and green leafy vegetables. Consider making a simple smoothie with high-fiber fruit, fresh spinach and milk.
- consider higher-fiber cereal with 8-10g fiber/serving as long as it’s given with plenty of fluids.
- rule of thumb: fiber found in food is better than fiber gummies or supplements.
- avoid constipating foods, including starches (pasta, potatoes, rice, crackers, bread, etc), bananas, cheese and excess milk intake.
- for kids over 12 months, do not give more than 24 oz milk/day.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- has severe pain and the above measures give no relief, or if you see a large amount of blood in the stool.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- has recurrent constipation or accidents related to withholding.
- has a small amount of bleeding after stooling.
COVID-19
COVID is a viral respiratory infection with symptoms of variable severity. In general, the care for a child with COVID is supportive care. As with all infections, it is important to keep your child well-hydrated and provide a comfortable place to rest. You can clear nasal secretions to help your child to more comfortably breathe. Please see the LA County Department of Public Health (publichealth.lacounty.gov) and CDC (cdc.gov) for current information.
CROUP
Croup is a response to an infection that results in noisy inspiration (breathing in), hoarse voice and a cough that sounds like the bark of a seal. Croup is usually caused by a virus that causes swelling near the vocal cords. This occurs during the night in children under 6y. It tends to show up suddenly in the middle of the night, when children awaken suddenly with very noisy breathing, painful cough and are often frightened. After the croup resolves, your child may have cold symptoms for several days.
What you can do
- Keep your child calm.
- Go into the cool night air for 5-10 minutes to help breathing (an open freezer door may work as well). A possibly less effective option is to run a steamy shower and sit in the bathroom to breathe the steamy air or use a humidifier.
- If your child is still having a difficult time, take a drive in the car with the windows down towards the nearest emergency room (dress appropriately). IF THERE IS NO IMPROVEMENT, GO INTO THE EMERGENCY ROOM.
- Once your child is calm, keep the room cool and humid (a humidifier may help).
- Sleep near your child so that you can assess their breathing throughout the night.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- has severe croup symptoms and you cannot control the symptoms.
- your child is sitting up, leaning forward, drooling, has their chin jutting out and looks quiet. This may be a very rare condition called epiglottitis, which is an extreme emergency.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- has had a difficult first night.
- is still having noisy breathing during the day.
- has croup that is not improving after a few nights.
- has croup that comes on after a week of a cold.
EARACHE
Earache from a middle ear infection is often associated with a sudden onset of severe unilateral ear pain, often associated with cold symptoms. In younger kids, earache is associated with a lot of fussing, crying and sleeplessness. Ear pulling in kids under 2y is NOT a reliable sign of ear infection - it’s often normal.
There are generally two types ear infection:
- Middle ear infection - usually associated with a cold or allergies. Drainage may occur if the eardrum ruptures (rare).
- Outer ear infection - usually occurs after swimming and results in an ear that is tender to the touch.
What you can do
- Treat discomfort with a pain reliever, such as acetaminophen or ibuprofen.
- Apply a warm compress to the ear.
- Elevate the head.
CALL DURING OFFICE HOURS FOR AN APPOINTMENT TO EVALUATE EARACHE.
FEVER
Fevers are helpful! Fever is an important tool our bodies use to help us fight off more serious infection. Many parents worry that fever is harmful, but fever is actually helpful in preventing more serious illness. Normal fevers of 100-104 are actually good for children (exception in infants under two months of age), and higher fevers over 104 that our bodies generate do not cause brain damage. In general, your child’s symptoms and how sick your child looks and acts is much more important that the actual temperature.
Fever is defined as:
- rectal, forehead or temporal artery temperature of 100.4 (38 C) or higher
- under the tongue temperature of 100 (37.8) or higher
- armpit temperature of 99 (37.2) or higher - this tends to be an inaccurate way to measure
- ear temperatures tend to be inaccurate in children
A few facts about fever:
- Fever is your body’s way of fighting against serious infection. Many febrile illnesses in kids are viral. When we get a fever with a viral infection, our body is trying to prevent bacterial growth/infection.
- Fevers with infections don’t cause brain damage. Fevers from being in very hot air temperature can cause brain damage and require immediate medical attention (heat exhaustion or heat stroke).
- High fever doesn’t cause a seizure. About 2-4% of children under 6y can have seizure with fever. These seizures, while frightening to watch, generally last less than five minutes and do not cause permanent harm. Febrile seizures require a discussion with your physician.
- High fevers do not be treated or brought down. Sometimes kids can look very sleepy and out of it with a higher fever, but this resolves when the fever comes down. In general, treat with acetaminophen or ibuprofen only for misery or discomfort or if you are trying to understand if your child is truly lethargic.
- Fever will go up and down throughout the day. Commonly, kids will have highest fevers in the late afternoon and night. Fever is generally thought to be resolved once your child has had 24h without fever without use of a fever-reducer.
What you can do
Children under two months of age:
In infants under 2 months, any fever is concerning and requires immediate medical attention. Infants should have their temperature taken rectally only - other methods are not accurate. Make sure your baby isn’t overdressed, as this will sometimes raise the temperature. Do not give any fever reducer to children under 2 months of age. Infants can also be very ill without having a fever - if your child is lethargic or sleepy (eg. you are unable to wake the baby for 2 feedings in a row) or irritable (eg. you are unable to console your baby despite a variety of attempts) or is having difficulty breathing or just doesn’t look or seem right to you, you should call your doctor immediately.
Children over two months of age:
Remember, fever is one of the good guys, so don’t suppress it unless your child is miserable or in pain. You may administer acetaminophen (Tylenol) or, if your child is over 6 months of age, ibuprofen (Advil) for pain or discomfort.
IMPORTANT: NEVER USE ASPIRIN FOR CHILDREN UNDER 18 YEARS OF AGE!
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- is extremely irritable or lethargic and does not improve after acetaminophen or ibuprofen.
- has difficulty breathing.
- has a stiff (not sore) neck
- has a spreading purplish rash.
- has a seizure (convulsion). If your child has a seizure that lasts more than 5 minutes, call 911.
- has a temperature over 105.5 taken rectally (this does not necessarily mean a more serious illness, though).
CALL DURING OFFICE HOURS IF YOUR CHILD:
- is not improving after 48-72h of fever.
- is becoming increasingly fussy.
- you are concerned.
DIAPER RASH
Diaper rash has many causes.
What you can do
Irritant diaper rash:
This is the most common type of diaper rash, often from stool or urine. This results in areas of redness or raw skin that tends to spare the folds of the skin. It also frequently occurs when a child has diarrhea.
- protect the skin with large amounts of petroleum jelly (Vaseline). The more the better!
- if the rash is persisting/worsening, apply a thick layer (“like frosting on a cake”) of original Desitin (40% zinc oxide, “purple container’) or other barrier cream containing at least 25% zinc oxide. Reapply liberally every diaper change.
- do not wipe the skin if it is very raw. Instead, rinse off the stool in the sink or tub to avoid further friction or irritation.
- try to give “air time” without the diaper as much as possible to help the rash to heal.
Yeast diaper rash:
This tends to be a red, bumpy rash that thrives in the folds of the skin. It commonly begins a few days after an irritant diaper rash and is typically redder, angrier and has small red dots and bumps spreading out from the main rash. It may be itchy.
- try miconazole nitrate 2% vaginal yeast cream (eg. 7-day Monistat) or clotrimazone 1% cream 3x/day until the rash is gone for 2 days. Apply a layer of diaper cream over the anti-fungal cream.
- if the skin is raw, cover miconazole cream with a thick layer of diaper ointment.
- try to give “air time” without the diaper as much as possible to help the rash to heal.
If your child is prone to recurrent diaper rashes:
- apply a thin layer of petroleum jelly with each diaper change, even if there isn’t a rash.
- change diapers promptly.
- avoid dyes and fragrances that may be in wipes, diapers, soaps and detergents.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- is not improving with the above measures.
DIARRHEA
Diarrhea is a condition that causes our body to make many watery bowel movements per day. The most common cause is viral infection, can be associated with vomiting and can last up to two weeks. If diarrhea and vomiting occur together, it is important to treat the vomiting first (see Vomiting section). Some cases of diarrhea are caused by dietary choices, such as excess juice or fruit consumption.
What you can do
For infants:
- give breastmilk and/or Pedialyte or similar oral rehydration solution.
- give more fluid than typical to help replace the fluid losses.
- if your child is on formula and the diarrhea is persistent, you may need to switch to a lactose-free formula for a week or so.
- if your child takes solids, offer plain cereal with water, boiled potatoes, pasta or banana.
- probiotics may be useful.
- gradually return to a normal diet, but do not give a lot of fructose-containing foods (fruits).
For toddlers and older kids:
- give Pedialyte or similar oral rehydration solution (plain, grape, cherry or apple are preferred).
- choose foods such as chicken broth with noodles, rice, potatoes, crackers, bread, bananas, lean meats or proteins.
- avoid high fat foods, spicy foods, dairy (except yogurt) and concentrated sugars such as fruit juices.
- probiotics may be useful.
Diarrhea may last for days and generally should resolve on its own if you are able to keep up with fluid losses and stools are gradually improving.
CALL IF YOUR CHILD:
- appears to be dehydrated, with signs such as decreased urination, glassy eyes, lethargy, dry mouth, no tears, sunken eyes and/or soft spot.
- has stools that are bloody or very mucousy.
- has diarrhea that lasts longer than a week.
- has over 10 large liquid stools per day.
HEAD INJURIES
Head injuries are frequent and common, especially in young children. Most only require close parental observation.
What you can do
- observe your child carefully for changes.
- use an ice pack or cold pack in short intervals to reduce swelling.
- wake your child every 2h for the next 24h to see if they react normally to you.
- monitor for headache, nausea, fatigue, trouble concentrating.
GO TO THE EMERGENCY DEPARTMENT IF YOUR CHILD:
- loses consciousness.
- is dazed or very sleepy.
- has vomiting.
- is persistently crying or irritable.
- seems off-balance.
- if the skull is dented in (not a bump).
CALL DURING OFFICE HOURS IF YOUR CHILD:
- has headache, nausea, fatigue, trouble concentrating or if you suspect a concussion.
HIVES
Hives are a type of rash that is blotchy, red, irregular and itchy. They are commonly referred to as welts. They characteristically move around and change relatively quickly. Hives can last from minutes to weeks, but they will come and go in location over that time. They can be the first symptom in an allergic reaction to something - food, medication, allergens. They are also frequently associated with viral infections in children, and sometimes we don’t understand why they are happening at all.
What you can do
- oral cetirizine (Zyrtec) once daily will usually help stop the itchiness and diminish or clear the rash temporarily.
- make note of any new exposures and stop exposure to anything you suspect might be involved: medications, foods or other possible allergens.
- take serial photos to show your doctor.
CALL 911 IF YOUR CHILD:
- has hives associated with hoarseness, difficulty breathing, generalized swelling or weakness.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- there are water-filled blisters along with hives.
- has redness or swelling of the mucus membranes, such as the mouth.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- is on an antibiotic or medication that you stopped because of the hives.
- you are wondering if it might be related to a food allergy.
- the hives are lasting for days or are associated with other worrisome symptoms.
INFLUENZA (THE FLU)
The flu (influenza) is a viral respiratory infection that typically has a very characteristic abrupt and sudden onset of severe lethargy, weakness and sleepiness accompanied by high fever. Unlike the gradual onset of a cold, flu symptoms are very sudden and intense. The first 48h are usually spent sleeping, with headache, muscle aches and weakness. Over the next couple of days, the fever continues but the child is less sleepy, but typically with increasing congestion and cough with persistent muscle aches and weakness. Many patients develop wheezing (whistling exhalation). The congestion, cough and weakness slowly resolve over the next 2-4 weeks. Influenza A tends to be more severe in early symptoms; influenza B tends to be overall milder but with longer-lasting fever and more muscle aches (especially in the calf muscles).
Flu is NOT a cold with a fever. It is NOT gradual. It is NOT a vomiting/diarrheal illness (i.e. “stomach flu”), though sometimes people vomit with influenza infection.
What you can do
Call the office for evaluation. If diagnosed in the first 48h, an antiviral medication can be initiated that may shorten the course of illness.
- REST! Rest! Rest!
- Keep hydrated. Give a lot of fluids, including water, electrolyte drinks (eg. Pedialyte, Gatorade, etc), chicken soup, juices. Don’t worry too much if your child doesn’t want to eat much - the appetite will return when the child feels better. But fluids are very important.
- The fever is not harmful. It is ok to treat aching or pain with acetaminophen (Tylenol) or ibuprofen (Advil/Motrin).
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- has very difficult or very rapid breathing. Note: rapid heartbeat and rapid breathing are common with fever, so recheck when the fever is reduced.
- has chest pain.
- hasn’t urinated for 8 or more hours.
- is not arousable or is delirious.
- cannot keep down liquids or will not drink enough fluid.
- you suspect your child has the flu and you are worried that your child is extremely ill.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- you’d like a flu test in the first 48h to see if your child is eligible for an antiviral medication.
- your child has asthma or another chronic medication condition.
- the fever is not going away in 72-96h.
- the cough keeps getting worse after the first few days.
PAINFUL URINATION
Pain associated with peeing can be from several different causes. It can be due to irritation of the skin caused by chemical irritants (bubble baths, bath bombs, fragranced soaps), wiping too hard or not enough, sand or tight pants. It can also be due to a bladder infection. Bladder infections are often associated with frequent urination and a sense of urgency to urinate.
What you can do
- push fluid intake, including cranberry juice if possible.
- do clear water baths daily.
- if the skin is red, apply Vaseline generously.
SEEK PROMPT MEDICAL ATTENTION IF YOUR CHILD:
- has a fever.
- has a backache.
- is vomiting.
- looks ill.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- has symptoms that do not resolve with the above suggestions.
PINK EYE (CONJUNCTIVITIS)
Pink eye is inflammation of the eye caused by viruses, bacteria, allergies or irritants. The white of the eye is usually pink or red. Viral pink eye tends to have a mucousy or watery drainage that occurs mostly after sleep. Bacterial pink eye tends to have a more copious pus-like discharge that returns very quickly after wiping it away. Sometimes kids will wake up with their eyes sealed shut from dried discharge. Both viral and bacterial pink eye are contagious, but neither are emergencies.
What you can do
- clean eye discharge by using a damp cotton pad or soft cloth.
- if the eyes are very itchy, an over-the-counter allergy eye drop may help a little.
- do NOT use Visine or other eye drop to “treat” the redness.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- has severe eye pain.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- has pink eye that hasn’t resolved by the next morning.
SORE THROAT
Many conditions cause sore throat, including viruses, strep, sinus infections and allergies. Viruses cause the majority of sore throats. Strep throat is bacterial, needs to be diagnosed by a lab test and needs to be treated with antibiotics to prevent rheumatic fever.
What you can do
- Treat discomfort with a pain reliever, such as acetaminophen or ibuprofen. Popsicles and ice cream can be soothing, too!
- Encourage fluid intake. Again - popsicles! Soup works, too.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- has pain and swelling on one side of the throat and the other side is normal.
- cannot fully open their mouth.
- has difficulty breathing.
CALL DURING OFFICE HOURS IF YOUR CHILD:
- has a sore throat lasting more than 24h and is not associated with cough.
- has a sore throat with rash.
- has a very painful sore throat.
- has associated vomiting or abdominal pain.
SUNSCREENS AND INSECT REPELLANTS
The best way to prevent sunburns is to stay in the shade or use SPF-protective clothing. If this is not possible, apply broad-spectrum, water-resistant sunscreen with an SPF of at least 30 to your child’s skin. Sunscreens with the active ingredients of titanium dioxide or zinc oxide are preferred. Remember to reapply your child’s sunscreen at least every two hours or immediately after swimming or sweating. There is no such thing as “waterproof” sunscreen.
Insect repellants are one way to minimize mosquito bites. Some people tend to get more bites than others. The best way is to wear covering clothing and to avoid being outside during dusk, when mosquitoes are most actively biting. Also, look around your yard for areas of standing water where mosquitoes might lay eggs. If you would like to use an insect repellent, there are several forms. It’s important to read label directions carefully. The EPA website is a good place to review (epa.gov/insect-repellents/using-insect-repellents-safely-and-effectively).
In general, we recommend avoiding spray sunscreens and insect repellants whenever possible.
TESTICULAR PAIN
Testicular pain is usually of sudden onset and may be present with redness, swelling and a fever. It may be caused by viral infection or may be due to a twist in the base (root) of the testicle (this is called testicular torsion). Testicular torsion is an emergency and needs to be evaluated and corrected immediately to avoid permanent harm to the testicle.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD HAS TESTICULAR PAIN.
VOMITING
Don’t panic.
A day or two of recurrent vomiting in a child is often caused by a viral infection. In this circumstance, the stomach is very irritable and wants to throw everything out of it (vomiting). Your goal is to try to get as much fluid as possible to stay in your child’s body. Don’t rush to give your child fluids - wait until the vomiting has stopped for about an hour. Then start very slowly with very frequent but very small amounts of fluid, ideally Pedialyte or other oral rehydration solution - just enough to slip past the stomach to the intestine before the stomach kicks it out. If you give too much fluid too quickly, your child is more likely to vomit and become even more dehydrated.
What you can do
How to give fluids:
- give one teaspoon of Pedialyte or similar oral rehydration solution every 10 minutes for infants and every 5 minutes for older kids.
- if your child vomits again, wait about an hour and try again.
- if vomiting persists for a couple of hours, go ahead and give Pedialyte one teaspoon (5 mL) every 5-10 minutes.
- if the vomiting won’t stop, go to the ER.
- if your child can hold down Pedialyte one teaspoon 8-10 times, you can begin to give one tablespoon (15 mL) every 25-30 minute for infants and every 15 minutes for older kids.
- after an hour of this, very gradually give larger amounts of liquid.
- do not give over two ounces at a time for the first day.
- after six hours without vomiting, you can offer a bland and starchy diet - Saltine crackers, toast, banana, rice, chicken soup, etc.
- gradually return to a normal diet over next several days.
CALL THE DOCTOR IMMEDIATELY IF YOUR CHILD:
- appears dehydrated, with signs such as decreased urination, glassy eyes, lethargy, dry mouth, no tears, sunken eyes and/or soft spot.
- cannot stop vomiting or will not hold down even very small amounts of liquid at a time.
- has severe diarrhea (see Diarrhea section).
A WORD ABOUT ANTIBIOTICS
We get many questions about prescribing antibiotics over the phone. Please note that we do not prescribe antibiotics without proper evaluation and examination. Many illnesses in children are caused by viruses and antibiotics have no effect on such illnesses. However, if we have prescribed antibiotics for your child, please complete the course as prescribed to avoid antibiotic resistance. Probiotics (yogurt) can help if your child has diarrhea associated with antibiotics.
What if I need a refill of a prescription?
If you need a medication refilled, please call us during regular office hours. Please give us at least 24 hours notice for regular medication refills and at least 3 business days for triplicate medication refills. Please note that we do not refill prescriptions after office hours.